By Shelley Segal, CEO
The CMS report provides information on the program audit process, a current snapshot of the program audit landscape, and a summary of the 2021 program audits, as well as CMS’ enforcement actions.
The total number of currently-active sponsors audited between 2019 and 2021 is 42, or approximately 20 percent of the sponsors with currently active Medicare contracts. CMS conducted 27 audits in 2021.
2022 Part C and Part D Program Audits are happening now…. are you audit ready?
CMS imposed 16 Civil Money Penalties (CMPs) for referrals received in 2021 totaling $1,043,953 with an average of $65,247 per CMP. The highest CMP imposed was $146,068, and the lowest CMP imposed was $9,328.
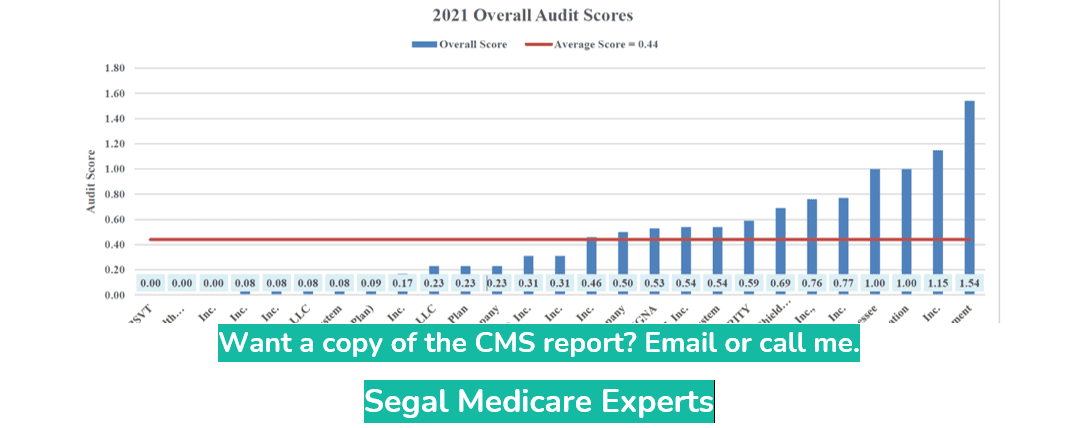
2021 Audit Results – The data analyses resulting from the 2021 program audits yield an average overall audit score of 0.44. Here is a graph of the 2021 Overall Audit Scores
Please contact us if you have questions, need more information about this guidance, or want a CPE Audit quote today:
Segal Medicare Experts
562.498.2218
segalmedicareexperts.com
